
Related Product

Reflux Relief System
$249.99 USD
Say goodbye to nighttime Acid Reflux & GERD pain without sacrificing comfort.
What Are Acid Reflux and GERD?
Share
Once you cross your mid-40s, a nice dinner doesn’t always stay “nice.” Instead of enjoying that pasta or taco, you might feel a fiery burn in your chest, like your food is staging a comeback tour. Sometimes it creeps back up the throat, leaving that bitter, sour taste nobody asked for. Yep, these are some of the typical acid reflux symptoms.
So, when you’re experiencing acid reflux, nothing is more important than relieving your symptoms. That unnecessary heartburn, a bitter taste in the mouth, and other symptoms of acid reflux can disrupt more than just your digestion. They can affect your comfort at home, your focus at work, and your overall quality of life. That’s why it’s essential to understand how to manage acid reflux early before it starts interfering with your health, productivity, and well-being.
In this post, we will try to understand “What is acid reflux?” and “What causes acid reflux?” We will also discuss the nuanced differences between acid reflux and GERD.
What is Acid Reflux?
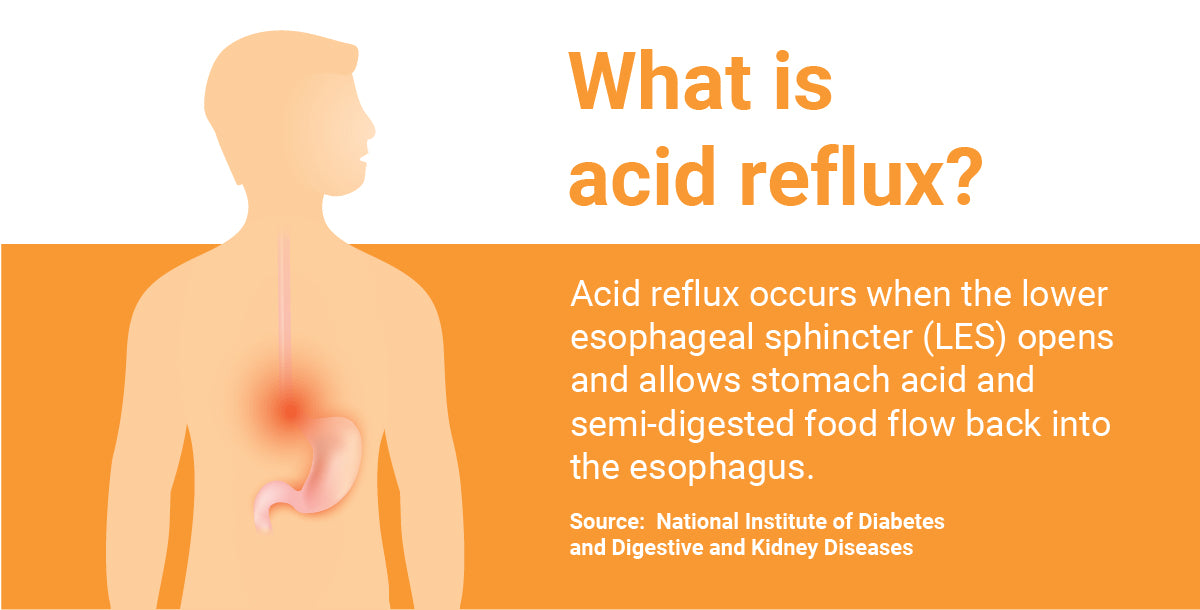
Acid reflux is a condition where stomach acid flows back into the esophagus, the tube that connects your mouth to your stomach. Usually, a small muscle at the end of the esophagus keeps food and stomach acid in. When this muscle weakens or relaxes at the wrong time, acid can move upward. This backflow often causes a burning sensation in the chest, commonly called heartburn.
Right above your stomach is a small valve called the LES, or lower esophageal sphincter. Usually, the LES only opens to let food in and air out (a.k.a. burps). For most people, acid reflux occurs when the LES opens and lets stomach acid and semi-digested food flow back into the esophagus.
-
It causes symptoms like heartburn, chest discomfort, regurgitation, and a bitter taste.
-
It can worsen after large meals, lying down, or eating spicy/fatty foods.
-
Frequent acid reflux may develop into GERD (gastroesophageal reflux disease), a more serious condition.
A report by the National Institute of Diabetes and Digestive and Kidney Diseases found that more than 25% of the people in the US suffer from GERD and Acid Reflux.
Heartburn (which has nothing to do with the heart) is among the major acid reflux and GERD symptoms and is caused by the acid eating away at the lining of the esophagus.
What Causes Acid Reflux?
Acid Reflux (GER) and GERD occur when your lower esophageal sphincter does not function properly, allowing stomach contents, like stomach acid, to rise and permeate the esophagus.
Several factors can trigger or worsen this condition, such as:

-
Overeating: Large meals put pressure on the stomach.
-
Certain foods and drinks: Spicy foods, fatty meals, citrus, tomatoes, chocolate, coffee, alcohol, and carbonated beverages.
-
Obesity: Extra belly pressure pushes stomach contents upward.
-
Lying down after eating: Makes it easier for acid to flow back.
-
Smoking: Weakens the LES and increases acid production.
-
Medications: Some painkillers, muscle relaxers, and blood pressure drugs.
-
Hiatal hernia: A condition where part of the stomach moves above the diaphragm.
-
Pregnancy can cause acid reflux as well, called gestational acid reflux. The growing baby creates less room for your stomach, and the hormone progesterone causes muscles, like the LES, to relax.
In some cases, a pregnancy pillow may relieve nighttime acid reflux symptoms.

Acid Reflux Vs. GERD
As an acid reflux sufferer, you may be familiar with the acronym GERD; in fact, acid reflux is also known as GER, gastro-esophageal reflux. GERD stands for gastroesophageal reflux disease, which is the chronic form of acid reflux. If you experience acid reflux symptoms twice a week or more, you may actually be suffering from GERD.
Both acid reflux and GERD are commonly associated with heartburn, but there are a few key symptomatic differences to note when comparing Acid Reflux vs. GERD.
|
Aspect |
Acid Reflux (GERD) |
GERD (Gastroesophageal Reflux Disease) |
|
Definition |
A condition where stomach acid flows back into the esophagus occasionally |
A chronic and more severe form of acid reflux. |
|
Frequency |
Occurs occasionally, often after heavy meals or certain triggers |
Happens two or more times per week. |
|
Severity |
Usually mild and temporary |
Persistent, more intense, and can lead to complications. |
|
Common Symptoms |
Heartburn, sour/bitter taste in the mouth, regurgitation |
Frequent heartburn, chest pain, difficulty swallowing, chronic cough, hoarseness |
|
Duration |
Short-term, usually resolves with lifestyle changes or over-the-counter meds |
Long-term condition requiring medical diagnosis and ongoing management |
|
Complications |
Rare; usually none, if occasion |
It can lead to esophagitis, ulcers, Barrett’s esophagus, or esophageal cancer if untreated. |
|
Treatment |
Lifestyle changes, avoiding trigger foods, and antacids |
Lifestyle changes plus long-term medication (PPIs, H2 blockers) or surgery in severe cases |
Note: If you have acid reflux, you may taste stomach acid or partially digested food in the back of your mouth. However, not all individuals with GERD symptoms have heartburn.
Other GERD symptoms may include:
-
Bad breath.
-
Nausea.
-
Abdomen or chest pain.
-
Trouble swallowing.
-
Respiratory issues.
-
Vomiting.

Are Acid Reflux Symptoms and GERD Serious?
Everyone experiences acid reflux occasionally, and a single episode is usually nothing to worry about. However, when GERD flare-up symptoms occur more frequently, they can signal a more serious condition. Regular exposure of the esophagus to stomach acid can lead to irritation, inflammation, and long-term complications if left untreated.
Over time, lingering acid causes inflammation and can create a precancerous condition known as Barrett’s Esophagus. That’s not meant to scare you, but it’s important to understand what is Acid Reflux and what treatment measures you can take to be proactive.

Acid Reflux Treatments
The three mainstream ways to treat acid reflux/GERD are
-
Lifestyle Changes
-
Medication
-
And surgery
Lifestyle changes are always the first consideration. If that doesn’t work, your doctor may recommend over-the-counter or prescription medications. As a last resort, acid reflux surgery may be necessary.
Lifestyle Changes
1. Avoid trigger foods:
Common trigger foods include citrus fruits, onions, garlic, tomato products, spicy dishes, fatty or fried foods, chocolate, peppermint, caffeine, and alcohol. However, not all of these may affect you, and other foods might cause symptoms. It often takes trial and error to identify your personal triggers.
2. Incorporate GERD diet foods:
Some foods can trigger acid reflux and GERD flare-up symptoms, while others may help reduce them. High-fiber foods, alkaline options like melons, bananas, and cauliflower, and water-rich foods such as cucumber, lettuce, watermelon, and broth can ease symptoms. Natural remedies like milk, apple cider vinegar, and ginger may also provide relief.
3. Lose weight:
GERD is more common in people who are overweight or obese, and weight loss can be an effective way to reduce or even resolve GERD symptoms
4. Adjust mealtime habits:
By changing how you eat, you may find relief from acid reflux. Try smaller meals, avoid eating right before lying down, eat slowly, limit fluids during meals, drink water between meals, take short walks after eating, and chew non-minty gum to aid digestion.
5. Sleep on an incline:
Elevating your head and upper body while sleeping uses gravity to keep stomach acid in place. This simple change can greatly reduce nighttime GERD symptoms, protect the esophagus from irritation, and improve sleep quality.
Medications
-
Antacids: Give quick relief by neutralizing stomach acid (Tums, Maalox). Best for mild, occasional symptoms.
-
H2 Blockers: Reduce acid production and last longer than antacids (Pepcid). Useful for mild to moderate GERD.
-
PPIs: Strong acid reducers that also heal esophageal damage (Prilosec, Nexium). Often used for persistent GERD.
-
Prokinetics: Help food move through the stomach faster, lowering reflux risk. Less common due to side effects (Reglan).
Surgery
-
Fundoplication: Strengthens the valve between the stomach and esophagus to block reflux.
-
LINX Device: A magnetic ring around the esophagus prevents acid backflow, allowing food to pass.
-
Endoscopic Procedures: Minimally invasive methods that tighten or reinforce the esophageal sphincter.
Can Sleeping Inclined Really Reduce Acid Reflux?
Yes, sleeping on an incline is an effective way to reduce acid reflux exposure during the night. When the upper body is elevated, gravity helps stomach acid stay in place and prevents it from flowing back into the esophagus.
Studies show that acid clearance time, the time it takes the body to naturally clear acid from the esophagus, can improve by up to 71% in this position. Sleeping inclined not only reduces reflux episodes but also helps protect the esophagus and promotes more restful sleep.
Looking for a Natural Way to Sleep Better with Acid Reflux? (new added subhead)
If you experience persistent acid reflux symptoms, it may be a sign of GERD that requires proper treatment. Choose MedCline’s Acid Reflux Relief sleep system that goes beyond reducing acid reflux to helping you sleep soundly and comfortably. Over the years, we’ve listened closely to feedback from physicians and reflux sufferers to develop the most effective, comfortable, and practical treatment possible.

Wrapping Up
Acid reflux occurs when the LES opens and lets stomach acid and semi-digested food flow back into the esophagus. GERD is the chronic form of gastroesophageal reflux. GERD symptoms may or may not include heartburn, in addition to bad breath, nausea, abdominal or chest pain, trouble swallowing, respiratory issues, and vomiting.
The three main treatment approaches are:
-
Lifestyle changes such as losing weight, adjusting diet, and sleeping at an incline.
-
Medications to control acid production and heal damage. (If medications don’t work, it’s worth learning the difference between GERD and NERD before consulting your doctor.)
-
Surgery is a last option when other methods fail.
Sleeping on an incline, especially on your left side, is one of the most effective ways to manage nighttime reflux. Elevating the body helps gravity move residual acid back into the stomach, reducing irritation and improving sleep quality. However, if you struggle with nighttime acid reflux, our Acid Reflux Relief System can help you get back to sleeping comfortably, reflux-free.

Related Product

Reflux Relief System
$249.99 USD
Say goodbye to nighttime Acid Reflux & GERD pain without sacrificing comfort.
