
Related Product

Reflux Relief System
$249.99 USD
Say goodbye to nighttime Acid Reflux & GERD pain without sacrificing comfort.
What to Consider Prior to GERD Surgery
Share
For some acid reflux and GERD sufferers, surgery is an option that is carefully considered with your doctor after all other possible solutions have failed to remedy the reflux. It’s not a decision that’s taken lightly. As with any surgery, there are risks involved, and, unfortunately, the most commonly used surgical procedure doesn’t always guarantee long-term results.
To help you determine whether GERD surgery is right for you, we’ve created this GERD-surgery guide that walks you through how to manage GERD without surgery, the different types of GERD surgery, and what to expect before and after GERD surgery. As always, it’s best to consult with your doctor to determine the right path to take to manage your acid reflux. With this guide, you can go to your doctor with information and questions that can help you determine the right course of action.
- What is GERD?
- Ways to manage GERD without surgery
- When is GERD surgery necessary?
- What is the best surgery for GERD?
- How much does surgery for GERD cost?
- What to expect before GERD surgery
- How is surgery for GERD performed?
- What to expect after GERD surgery
- Wrapping up: What to consider before surgery
What is GERD?
GERD, short for gastroesophageal reflux disease, is a form of bad acid reflux where the lower esophageal sphincter (LES) opens up, allowing stomach acid and partially-digested food to flow back into your esophagus1. Due to the stomach acid re-entering the esophagus, sufferers of GERD and acid reflux may experience uncomfortable symptoms, such as heartburn, coughing, chest pain, regurgitation, and difficulty swallowing.
Ways to manage GERD without surgery
For many, the thought of surgery can be stressful, overwhelming, and scary. Often, surgery is used as a last-ditch resort because it can be painful and expensive. Finding ways to combat medical issues without surgery is often recommended. Fortunately, there are a few ways you can manage the symptoms of GERD without surgery 2:
- Avoid trigger foods 3: Knowing what causes acid reflux flare-ups can help you manage GERD, such as trigger foods that are spicy, citrusy, or acidic, along with carbonated beverages.
- Eat GERD diet foods 3: While some foods can trigger GERD, others that can soothe and minimize the effects of GERD, such as high-fiber foods like bananas, watery foods like cucumbers, and milk.
- Weight loss 4: By losing weight, you can take off pressure from your abdomen, which can lessen the likelihood of stomach acid leakage or backflow.
- Sleeping position: GERD symptoms are often felt at night, leaving many wondering, “is it bad to sleep on your stomach?” In most cases, yes. Instead, it’s recommended to elevate your head to allow gravity to run its course and keep stomach acid at bay. MedCline’s Reflux Relief System creates an inclined, left-sided sleeping position for natural acid reflux relief.
- Medicine: For some, acid reflux medicine and over-the-counter medications, such as antacids, can help to reduce the amount of stomach acid your body produces.
When is GERD surgery necessary?
When any of the aforementioned remedies or other medical treatments don’t prove successful, surgery might be the next choice for those suffering from severe and chronic GERD. When left untreated, GERD and severe acid reflux can have some serious health complications, such as bleeding, esophageal scarring, ulcers, and esophagitis5.

What is the best surgery for GERD?
If your doctor determines that surgery is the best option to manage your GERD, it’s important to know what types of acid reflux surgery you can expect. Below are different GERD surgeries your doctor might recommend:
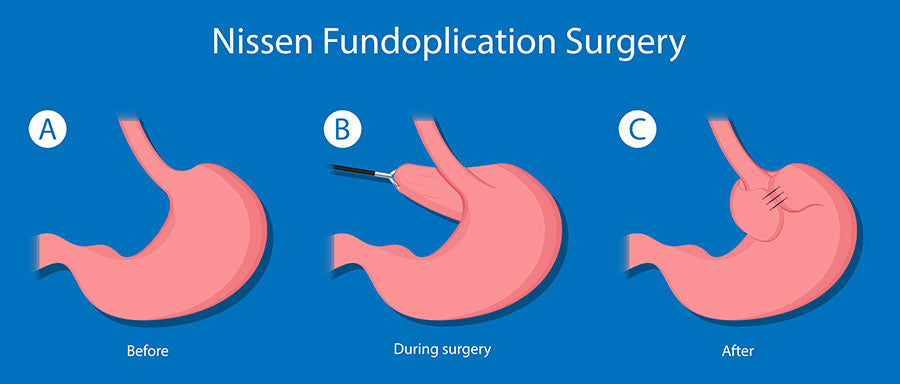
- Fundoplication: This is the most common GERD surgery. Through fundoplication6, your surgeon wraps the upper part of your stomach around the outside of your lower esophagus, which strengthens the sphincter.
- Transoral Incisionless Fundoplication (TIF): When open fundoplication can’t be performed, TIF7 is used instead. This procedure is performed with the EsophyX device, which is inserted through your mouth, creating a new valve at the base of your esophagus to help reduce GERD. For those looking for a less invasive acid reflux surgery, talk to your doctor about TIF.
- Stretta Procedure: The Stretta Procedure8 delivers radiofrequency energy to your esophagus through an endoscope. The electrodes on the tube deliver heat, which creates small cuts on your esophagus. When these cuts heal, they form scar tissue, which can help strengthen esophageal muscles and block nerves that respond to acid reflux.
- Bard EndoCinch System: This system isn’t widely used and not always covered by insurance, but still worth mentioning to your doctor. The Bard EndoCinch System9 uses an endoscope and sews stitches horizontally to create pleats in the LES to help strengthen it.
- Linx Surgery: The Linx Reflux Management System10 is a small flexible band constructed with titanium beads in the shape of a ring and is implanted around the lower end of the esophagus to restore your body’s natural barrier to reflux. This heartburn surgery is relatively non-invasive and takes less time than traditional surgery.
When it comes to determining the best surgery for GERD, it’s important to consult with your doctor. They will be able to give you informed advice and can help you work with your insurance provider to find the most cost-effective and reliable option.
How much does surgery for GERD cost?
The price of GERD surgery depends on a few factors, such as:
- Your insurance coverage
- Location of your doctor
- The type of GERD surgery you get
- Your doctor’s experience
However, most estimates claim that GERD surgery’s price can run anywhere between $3,000 and $5,00011.
What to expect before GERD surgery
For anyone, going under the knife can be a nerve-racking experience. Knowing what to expect before acid reflux surgery can help give you peace of mind. When getting surgery for acid reflux12, in most cases fundoplication, this is what you can expect:

- Your surgeon will conduct a full-body assessment to assess whether you pose any potential risks and determine whether you’re a good candidate for heartburn surgery.
- Once you go over potential risks, you will provide written consent for GERD surgery to be performed.
- Your surgeon will then conduct blood work, take a chest X-ray and an EKG (when applicable), and perform a medical evaluation.
- In some cases, you may need prior surgery or tests before getting GERD surgery based on your medical history.
- Your doctor will ask you to avoid eating or drinking anything besides prescribed medications the night before your GERD surgery.
- Avoid taking aspirin, blood thinners, Vitamin E, and any other anti-inflammatory medications several days or weeks before surgery.
- On the day of surgery, a nurse will inject a small needle or catheter into your vein to deliver medication.
- The surgeon will use general anesthesia to put you asleep during the operation.
- Once the operation is complete, you will be sent to the recovery room until you are fully awake.
- In some cases, you may be required to stay in the hospital overnight or for multiple days.
How is surgery for GERD performed?
Currently, the most popular surgery for GERD is a Nissen fundoplication13. In this procedure, the stomach’s upper portion is wrapped around the esophagus and sewn into place. The result is that the lower portion of the esophagus passes through a small tunnel of stomach muscle. This helps to stop stomach acid from getting back into the esophagus as the valve between the esophagus and stomach (lower esophageal sphincter or LES) is made stronger. The absence of acid helps the esophagus to heal from previous damage caused by repetitive acid exposure. The surgery is either performed through a large incision or laparoscopically.
What to expect after GERD surgery
Depending on how the surgery is performed, you’ll be in the hospital anywhere from two days to several days. Most people go back to work between a couple of weeks and six weeks following their operation, depending on the method of surgery, the type of employment they have, and how well the recovery is going. Some people bounce back quickly while others find their bodies need more time to heal. In any case, a post-surgery recovery pillow may help to alleviate discomfort during your period of bed rest.

After surgery, you may need to change how you eat. Your diet may consist mostly of soft foods until your body recovers. You may find that food needs to be chewed more thoroughly and that you need to eat more slowly in order to give food enough time to move down the esophagus.
A positive outcome of fundoplication surgery is that the esophagus heals without the daily assault of stomach acid. While most people initially see an improvement in GERD, almost half of the patients either had symptoms return, had esophagitis (inflammation of the esophagus), required medication for symptoms, or needed another operation after seven years.
For some, the side effects of surgery are as troublesome as GERD. There can be bloating caused by gas buildup, swallowing problems, and internal pain where the surgery was performed. It’s impossible to predict who will have complications, and the fundoplication procedure cannot be reversed.
Like with many surgical solutions, alternative procedures are evolving and becoming more readily available. For example, the new LINX Reflux Management System14 is gaining attention as the procedure is less invasive and takes as little as 25 minutes. A device is implanted into the lower end of the esophagus that consists of weakly magnetized beads held in a ring on titanium wire. The beads separate to allow food and drinks to move into the stomach and then contract to keep stomach acid out of the esophagus.
Based on clinical trials, the results have been positive, with more than half of the patients experiencing no symptoms after six months. However, as with most surgeries, there are possible side effects as 15% reported feeling something when they swallow, and 5% have difficulty swallowing once a day, six months following the procedure.
Wrapping up: What to consider before surgery
While surgery can be successful for some in resolving acid reflux, for others, the solution is only temporary or creates other unpleasant symptoms. That’s why it’s essential to give lifestyle changes a fair chance. Many people have found relief simply by sleeping on an incline15. In fact, of all the possible lifestyle changes, this is one of two that’s supported by clinical data (the other being weight loss).
But don’t just take it from us – sometimes it helps to listen to others who are going through a similar experience. We are fortunate to have heard from acid reflux/GERD sufferers who have used our incline system and have had real results. Here are a few of their stories:
- “Even when I was taking Ranitidine every day, I was still getting lots of reflux. After using MedCline for three nights, my reflux just went away and hasn’t come back.” Bill C. Age 66, California, Throat Cancer Survivor
- “I have not felt this good in ages. MedCline is magic!” Kelt M. Age 44, Michigan
- “Excellent product! MedCline has dramatically reduced my nighttime symptoms. In the three weeks I’ve been using it, I’ve been able to reduce the use of my prescription GERD medication by more than half, and I’m expecting to soon be able to eliminate it entirely.” Mark K., DDS Age 74, California
- “I love my MedCline! I’ve only taken Zantac once since I began using it. When I eat foods that I know I shouldn’t, it lets me sleep without any reflux. It seems to be lessening the frequency of my nighttime flare-ups as well.” Amber Y. Age 31, Wyoming
- “MedCline is an amazing product. It got rid of my pregnancy GERD symptoms and helped to support my back and stomach so I could finally get a good night’s sleep.” Adele W. Age 34, California
- “I have been waking up almost every other night since I was sixteen with acid reflux. In the first two months of using MedCline, I only woke up once.” Austin L. Age 20, Idaho
When you are deciding between surgery and other approaches to relieving your acid reflux, consult your doctor and consider all the costs, risks, and potential complications of the surgery. Then think about the same with medications and lifestyle changes and decide which approach—or which combination of treatments—makes the most sense for you.
At MedCline, our Reflux Relief System consists of a patented three-component Sleep System that creates the doctor-recommended inclined, left-side sleeping position to provide natural acid reflux symptom relief. With three available sizes and a patented arm pocket for your downside arm, our Reflux Relief System can help alleviate the uncomfortable symptoms of GERD and acid reflux.
References:
- “Definition & Facts for GER & GERD,” National Institute of Diabetes and Digestive and Kidney Diseases, https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/definition-facts
- “Surgical Treatments,” International Foundation for Gastrointestinal Disorders, https://aboutgerd.org/treatment/surgery/surgical-treatments/
- Gupta, Etka, “GERD Diet: Foods That Help with Acid Reflux (Heartburn),” Johns Hopkins Medicine, https://www.hopkinsmedicine.org/health/wellness-and-prevention/gerd-diet-foods-that-help-with-acid-reflux-heartburn
- “Weight Loss Can Lead to Resolution of Gastroesophageal Reflux Disease Symptoms: A Prospective Intervention Trial,” U.S. National Library of Medicine National Institutes of Health, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3853378/
- Clarrett, Danisa M, and Christine Hachem. “Gastroesophageal Reflux Disease (GERD).” Missouri medicine vol. 115,3 (2018): 214-218. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140167/
- Anti-Reflux Surgery, MedlinePlus.gov, https://medlineplus.gov/ency/article/002925.htm
- Fass, Ronnie. “An Overview of Transoral Incisionless Fundoplication and Magnetic Sphincter Augmentation for GERD.” Gastroenterology & hepatology vol. 13,1 (2017): 50-52. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5390325/
- Triadafilopoulos, George. “Stretta: a valuable endoscopic treatment modality for gastroesophageal reflux disease.” World journal of gastroenterology vol. 20,24 (2014): 7730-8. doi:10.3748/wjg.v20.i24.7730, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4069301/
- Mahmood, Z et al. “Endocinch therapy for gastro-oesophageal reflux disease: a one year prospective follow up.” Gut vol. 52,1 (2003): 34-9. doi:10.1136/gut.52.1.34, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1773510/
- The LINX Reflux Management System, Medical College of Wisconsin, https://www.mcw.edu/departments/surgery/divisions/minimally-invasive-and-gastrointestinal-surgery/patient-care/gerd-and-gastrointestinal-surgery-program/gastroesophageal-reflux-disease-gerd/the-linx-reflux-management-system
- Carlson, Joe. “Device for acid reflux approved by FDA, but not insurers.” Star Tribune (2016), https://www.startribune.com/device-for-acid-reflux-approved-by-fda-but-not-by-insurers/303946711/?refresh=true
- “Anti-reflux (GERD) surgery patient information from SAGES,” SAGES, https://www.sages.org/publications/patient-information/patient-information-for-laparoscopic-anti-reflux-gerd-surgery-from-sages/
- Heartburn/GERD Health Center, Fundoplication Surgery for Gastroesophageal Reflux Disease (GERD), (August 5, 2010), https://www.webmd.com/heartburn-gerd/guide/heartburn-surgery
- Lucas, Christine. “Savannah doctor pioneers surgical treatment for severe acid reflux,” SavannahNow, (January 12, 2013) https://www.savannahnow.com/story/news/2013/01/12/savannah-doctor-pioneers-surgical-treatment-severe-acid-reflux/13518734007/#.UPmKcqWjTzI
- Khan BA, et al. Effect of bed head elevation during sleep in symptomatic patients of nocturnal gastroesophageal reflux. J Gastroenterol Hepatol. 2012 Jun;27(6):1078-82. https://pubmed.ncbi.nlm.nih.gov/22098332/
Related Product

Reflux Relief System
$249.99 USD
Say goodbye to nighttime Acid Reflux & GERD pain without sacrificing comfort.
